Expert advice on bed-wetting

Being dry all night seems an elusive dream in some households. We asked the experts for their advice on managing bedwetting.
Toilet training makes it into the 'top ten most talked about' topics for parents of young children, and bedwetting is regularly up for discussion. We asked Shannon Clement for her tips on working towards dry nights.
Timing
You can attempt night-time toilet training at the same time as daytime training, or you can wait until your child has mastered the toilet during the day before giving nappy-free nights a go. Some parents like to wait until they’ve observed a few consecutive nights of dry nappies. Others like to encourage readiness by transitioning from a night nappy to a heavy-duty training pant, such as the Grovia My Choice Trainer, so their child can feel the wetness when they urinate. Basically, it comes down to what you think will work best for your child. Some children respond well to the consistency of being nappy-free day and night right away. Other children take a little longer before they have the bladder capacity to hold on all night or the ability to wake in time to independently go to the toilet.
Tools of the trade
To help stay positive, you’ll need some protective bedding or draw sheets, such as a Brolly Sheet or the Protect-A-Bed Up and Under. These sanity-savers protect your child’s valuable mattress and can be removed for washing without having to remake the whole bed. As a mum of boys, I’m a big fan of the Up and Under, as it protects top sheets and blankets when the urine goes upwards. Older kids may be able to remove draw sheets by themselves, so you can make up the bed with two draw sheets and let your child manage any late night changes independently.
Support team
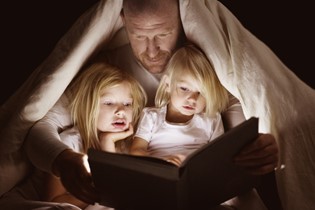
You can try a 'dream wee', where you get your child up during the night to take them to the toilet. Some children respond well to a bed-wetting alarm, like the Dri Sleeper, which goes off in time for your child to visit the toilet before a complete accident. It's also helpful to give your child a torch or ensure the way to the toilet is dimly lit at night.
Stay positive
As with daytime toilet training, punishment and negativity just don't work. Use lots of positive reinforcement and keep the process as stress-free as possible. Give your child encouragement for the helpful things they do on their journey to dry nights, such as avoiding drinks before bedtime, going to the toilet during the night or recognising when they’ve had an accident. Avoid showing your frustration over any wet beds. Children are all different – some will take longer to be dry all night than others, but they will all get there eventually.
Shannon Clement is a mum to two super high-energy boys.

Dr Anne Tait is a general paediatrician at Starship Children’s Hospital and Auckland Medical Specialists. She has an interest in all areas of children’s health and wellbeing.

AS FEATURED IN ISSUE 36 OF OHbaby! MAGAZINE. CHECK OUT OTHER ARTICLES IN THIS ISSUE BELOW